Owning Up to Medical Error
 by Danielle Ofri
by Danielle Ofri
Health Affairs Journal  (also in The Washington Post).
Precisely two weeks after completing my medical internship, I proceeded to nearly kill a patient. July marked the start of my second year of residency at New York City’s Bellevue Hospital, and it was my first time being fully in charge of a patient.
My patient arrived in fully developed DKA—diabetic keto-acidosis—a life-threatening condition in which lack of insulin causes a metabolic cataclysm. It was a classic Bellevue DKA patient story: arrested during a small-time drug deal, tossed into a New York City Police Department holding cell, unable to access insulin. The patient sat in the cell as his sugar wormed its way to stratospheric levels. When he began to vomit and his speech slurred, the police brought him to our emergency room (ER).
With my intern looking to me for guidance—he, with the ink still wet on his medical degree; me, with a scant single year more experience—I placed the patient on an intravenous insulin drip. DKA is one of those rare, gratifying conditions in which a patient arrives in extremis and, with deft handling of insulin, can be readily “cured.†I felt a surge of pride as we watched our patient gain consciousness, get cranky, demand double portions of food.
We were in a cramped, dingy corner of the ER next to the trauma bay, stuffed next to a narrow desk overflowing with x-rays, charts, coffee cups, and stethoscopes. Staff members perched there trying to conduct medical business, while paramedics wheeled in patients with shotgun wounds and survivors of motor vehicle crashes.
Within hours, our DKA patient’s glucose returned to normal. In triumph, I handed a “d/c insulin drip†order to the nurse because we no longer needed ongoing intravenous insulin. I was officially declaring our patient cured.
The nurse took the order from me, while passing a bottle of saline to another medical resident. “Do you want to give an injection of long-acting insulin before stopping the insulin drip?†she asked me, as the clerk pressed two more charts in her direction.
I thought for a moment. Why would I want to use the sledgehammer of long-acting insulin after eight hours of our meticulous adjustments with the insulin drip? “No,†I said, turning to my intern, capitalizing on the teaching moment. “If we push him overboard with long-acting insulin, it’ll be stuck in his system for hours, and his sugar could bottom out. Let’s just keep checking his glucose hourly and give him short-acting insulin as needed.â€
The nurse raised her eyebrows ever so slightly.
The intern nodded with me—my logic was obvious. The nurse shrugged and went back to her work.
My logic was, indeed, obvious. It was also wrong. Right-out-of-the-textbook wrong. The very thing you are supposed to do in DKA is administer long-acting insulin just before stopping the insulin drip. Otherwise the patient will turn right around and plunge back into DKA.
When the blood tests revealed dangerously rising levels of potassium and acid in his body, I panicked and paged the senior medical resident for help.
‘What Were You Thinking?’
My intern and I stood nervously while the senior resident scrutinized the numbers. She wrinkled her brow for perhaps three seconds, then shot me a withering look. “Didn’t you give him long-acting insulin before you turned off the insulin drip?†she demanded. “A little longer like this and he’ll be comatose! Next thing you know we’ll be calling a code for his cardiac arrest.â€
I tried to describe our methodical treatment and how logic would dictate—wouldn’t it?—that we shouldn’t muck up a tenuous situation with long-acting medications, that we wouldn’t want to harm the patient by pushing his sugar too low, that we…
My words began to run up against each other, progressively garbling under the weight of her granite stare until they petered off into silence. Another trauma case had just been wheeled in, and surgeons bustled past us, shouting competing orders.
“What were you thinking?†the senior resident said, her normally pleasant voice now like a drill sergeant’s.
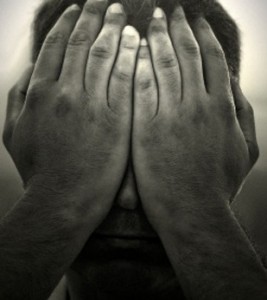
I stood there stone still as my brain cells slowly dissolved into muck.
“What were you thinking?†she repeated, her voice now thundering through the ER, despite the pandemonium swelling around us. Lives were at stake, left and right, and she clearly wasn’t going to let me get out of this.
I couldn’t even muster a whisper, knowing that my intern, who had nodded so trustingly at my earlier pronouncements, was standing not four inches from me. Scrub-clad bodies were jostling against me in the cramped space of the ER, but I felt a gulf widen around me, as though I’d just lost control of my bladder and was standing in a growing puddle of mortification.
What had I been thinking?
Had I simply forgotten the part about the long-acting insulin? Had I misread the textbook? Had I slept through the lecture on DKA? Was I simply not smart enough to be a doctor?
The senior resident stared at me, waiting for an answer. I knew I’d made a mistake, but this prolonged agony—thirty seconds clawed out to an eon—was not helping me know that awful truth any better.
If only my intern weren’t standing right next to me. Alone I could probably have handled the rightful reprimand, but the humiliation in his presence was unbearable.
The senior resident wrenched the pen from my hand, and furiously wrote orders to restart the insulin drip immediately, to administer long-acting insulin along with calcium and bicarbonate to avoid cardiac arrest from dangerously skewed potassium and acid levels. I thought she was going to wrench the patient out of my hands as well.
When she finally departed, I couldn’t even raise my eyes toward my intern. All I wanted was to crawl under a rock and weep. But I couldn’t. There was an intern waiting for guidance and a patient who needed medical care.
“Let’s, uh, check the patient’s fluid status,†I stammered, the heat in my cheeks making it difficult to articulate words, “and then draw another set of labs.â€
“Got it,†the intern said. Matter-of-factly he began tearing open gauze pads, pulling out alcohol swabs, labeling test tubes. It was the normalcy of his actions that allowed me to breathe again. The absolute ordinariness of his conduct was an act of compassion that I’ve never forgotten. We returned to our patient whom we were able to rescue—once again—from DKA. In two days he was back with the cops.
The senior resident graduated and went off to another job. The intern became a fine doctor in private practice. I continued an academic career at Bellevue. Since that day, I have never failed to inject long-acting insulin before stopping an insulin drip.
Lesson learned. Doctor reeducated; mistake never to be made again.
Patient did fine, suffered no ill effects. Near miss caught in time by the system of having more-experienced doctors supervise less-experienced doctors.
Case closed. Or should it have been?
The Shattering Effect Of Shame
Certainly, in those days, that’s how such near misses and errors were treated. If this had happened today, there might be a different ending to the story. If I’d been a medical resident now, the patient would have been approached by the medical team, and possibly risk management personnel, informed of a medical error that was potentially life threatening (despite being a “near miss†in terms of outcome), received an apology, and be told that the hospital and physician accepted full responsibility.
As a mature physician, I can accept this as the ethical thing to do. But as a fledgling doctor, humiliated down to the calluses on my feet, I couldn’t imagine anything more dreadful.
Taking responsibility wasn’t the hard part—I’d already spent weeks flagellating my brain for its incompetence. But the idea of dragging my sorry self into the patient’s room, looking him straight in the eye, and explaining that I’d committed a grave error because of my incompetence—one that threatened his life, one that kept him in the intensive care unit (ICU) for an extra day, one that exposed him to another day’s worth of ICU pathogens and procedural risks, not to mention cost—was humiliating beyond comprehension.
It seems entirely obvious: Doctors need to apologize for their errors, even if the patient got lucky and didn’t suffer irreparable harm. But in the real world of medicine, acknowledging responsibility is a dicey proposition. To most physicians it’s tantamount to handing your head to a lawyer on a surgical tray. This fear of lawsuits is so potent that even the most ethical physicians clam up when issues of medical errors arise.
Apologies can often be considered evidence of fault. Depending on the state where the error happens, there are some protections for apologies that express sympathy, but there is variation as to whether this extends to apologies that invoke responsibility for an error. Despite progress on this legal front, doctors fear that their apologies could be used against them, and they have little faith that legislation will protect them.
Typically, the most that doctors can muster is, “I’m so sorry this happened.†Such pseudo-apologies are taken to task by Aaron Lazare in his fascinating book, On Apology (Oxford University Press, 2004). They are meaningless, he writes, because they lack the key ingredient of acknowledging responsibility.
Lazare notes three emotions that influence the decision to apologize: empathy, guilt, and shame. Some doctors might lack empathy, but they have no trouble with guilt, even if they’d rather lick their wounds in private.
But then Lazare distinguishes carefully between guilt and shame. Guilt is usually associated with a particular incident and can dissipate when the issue is resolved. But shame reflects a failure of one’s entire being. Although guilt often prods a person to make amends, shame induces a desire to hide.
Shame, Lazare writes, is “an emotional reaction to the experience of failing to live up to one’s image of oneself.†Here, I believe, he puts his finger on the precise fiber of resistance in doctors.
When I think back to that moment in the ER when the senior resident berated me for my error, it was shame that overpowered me. Of course I felt guilty—that was the easy part. But it was the shame that was paralyzing. It was the shame of realizing that I wasn’t who I thought I was, that I wasn’t who I’d been telling my patient and my intern I was. Up until that moment, I’d thought I was a competent, even excellent, doctor. In one crashing moment of realization, that persona shattered to bits.
Addressing Shame
One could argue that this is a self-centered way of viewing the episode: how the doctor felt. After all, it was the patient who experienced the error. But it’s precisely the doctor’s emotions—particularly shame—that stand as the major impediment to the full-disclosure policies that are increasingly demanded.
Even if evidence convincingly demonstrates that disclosure and apology lead to fewer lawsuits, the desired culture of openness will come about only when we address the issue of shame. No matter how rational we doctors claim to be, the fragility of the human heart can prevail over data, ethics, and laws.
One has to wonder, then, why doctors feel our entire sense of self at risk when we admit errors. Perhaps the culture of perfection in medicine fosters a strictly binary analysis—you’re either an excellent doctor or a failure.
In most other aspects of life we seem to be able to accept the notion of “good enough.†But there is no room for the good-enough doctor. An error redounds not as a misstep that can be remedied with education, but as an intrinsic incrimination of one’s very being, not to mention a possibly dead or gravely injured patient.
Shame worms its way into the heart and is remembered like few other things. I’ll admit that the intricacies of DKA physiology have grown a bit fuzzy over the years. But the details of my insulin error in the dingy Bellevue ER are crisply stored in the linings of my heart. To this day, when I teach my students about DKA, I emphasize that clinical point with the vehemence of Moses on Sinai: “Thou shalt not turn off the insulin drip until long-acting insulin has been administered.â€
All medical training programs now include education about medical error. “Morbidity and Mortality†conferences have been largely shorn of their accusatory histrionics and now are rightly geared toward helping doctors learn from errors. But rarely is shame addressed. It seems so out of the realm of medical education—fodder only for those on the couch with their analyst.
But it is the elephant in the room. No doctor will easily confess to error when a core sense of self is at risk. It’s difficult to develop policy that addresses such a murky and uncomfortable issue as shame. But it wouldn’t hurt for the senior faculty—the chairs, the division chiefs, the master clinicians—to talk publicly to trainees about their own errors, and to specifically address how they dealt with the shame. The very fact of these doctors’ continuing to be doctors—highly successful ones—despite their errors and the attendant assaults on their egos, would itself be a potent lesson to the students and interns. It is possible to hold one’s head up after an error, to admit that errors are part and parcel of human existence, even in medicine. It is possible to see the error as an aspect of our self, but not the defining fundamental of our self.
Tending The Inner Landscape
A decade and a half after my DKA incident, I ran into that senior resident, having not seen her since our training. Ironically, perhaps prophetically, we weren’t brought together in the fellowship of doctorhood. We’d found each other, both hulkingly pregnant, in the waiting room of an obstetrician’s office. We chatted easily about jobs, spouses, families, career milestones.
Although our meeting now was a joyous one—colleagues reconnecting, the shared excitement of new lives about to begin—all I could see were the grimy, greenish walls of the Bellevue ER. I doubt if she even remembered that incident, but I couldn’t keep down the emotions of that long-ago error.
Easing the legal landscape with programs that fully disclose error is necessary but not nearly sufficient to foster openness about medical errors. It’s our inner landscapes that need to be tended to. Unless we can defuse the shame and loss of self that accompany admitting medical errors, there will always be that taut inner core of resistance.
Policy efforts have been directed toward proactive settlements with patients, and there is evidence that lawsuits are declining. But emotions can’t be legislated away. Even if these programs can coax physicians to come forward, the gut instinct to hide an error and defend the inner self will always be the first lynx to pounce on the heart.
from Health Affairs journal. (Also reprinted in the Washington Post).
