The Insanity of Recertification
 by Danielle Ofri
by Danielle Ofri
Slate.com
A year ending in a six is moving swiftly past us, and that can only mean one thing to a swath of the folks who carry stethoscopes in their pockets and happened to have finished residency in a similarly numbered year—it’s the decennial requirement to prove your worthiness as a physician.
When I completed my residency training in 1996, I crammed for the better part of a year and took the board exams that labeled me “board certified†by the American Board of Internal Medicine (ABIM), the certifying board for internists. While board certification in one’s field of specialty is not technically required in order to hang out a shingle in the United States—only a state medical license is needed—in practice, a doctor cannot get a decent job without it.
Board certification launched in 1936 with one single octopus of a test that you wrestled down at the end of your residency. If you survived, you were then dispatched into practice and never had to look back. In 1990, however, a monumental change occurred—board certification would no longer be a one-time event (except for the lucky pre-1990 cohort that was grandfathered in). Doctors would now have to retake the test every 10 years. And during the decade interim between tests, doctors would have to complete a certain number of educational credits in order to prove they were keeping up with the new knowledge.
This all made some sense, as medicine is continually changing, and we doctors owe it to our patients to keep up to date. When I recertified in 2006, there was a lot of material on the test that hardly existed in 1996. But a funny thing has happened. The “maintenance of certification†process, or MOC as it’s commonly known as, morphed into its own industry. In the 10-year interim between tests, ABIM and the other medical specialty boards began instituting ongoing requirements—online medical knowledge modules, practice improvement modules, projects that required getting evaluations from patients to prove your competency as a physician. Every few years another requirement sprouted and the fees increased commensurately.
As the requirements, stakes, and costs ballooned, tempers flared. Things reached a fever pitch two years ago when 20,000 doctors signed a petition in protest of the continued escalation of costs and requirements. The ABIM responded, though not as much as many critics had hoped: They acknowledged the dissatisfaction but the only substantive change was scrapping the paperwork-intensive patient evaluations.
Personally, I haven’t minded the ongoing modules, at least the ones that contain useful medical knowledge. Each module offers 30-odd clinical cases to evaluate. The modules take a few hours to complete, and they—like real-life medicine—are open-book. You can consult any journal, book, or database. You could do the whole thing with Wikipedia if you want, or you can call your med-school buddy with the photographic memory.
The clinical cases seem relevant enough to real life and they often force me to look up things I haven’t thought about for a few years, or clarify the specifics on something I only have a general sense about. I can sense loose globules of knowledge coalescing in my brain, and I feel like I am doing something salutary for my patients. In fact, in real life, when I see a patient with an issue that is even remotely outside of my immediate purview, I seek out the information rather than rely on my memory. Most doctors I know would consider it malpractice to rely on their fallible memories.
But then there’s the decennial exam. It is the kind of test where you have to surrender all belongings short of your skivvies and then depend on your memory for a grueling 10-hour exam. And it fills me both with dread and indignation. The dread is personal: Brute-force memorization is a skill for the lithe and the unencumbered. By the time you have a full-time job, a family, a mortgage, and eyes that must squint at smaller fonts, memorizing is an atrophying muscle.
The indignation, though, is professional. A half century ago, when board certification really came into its own, the scope of medical knowledge was in fact something that could hypothetically be memorized. The estimated doubling time of medical knowledge was in 1950 was 50 years. But that has speed up as science advances. In 1980 it was 7 years. In 2010 it was 3.5 years. By 2020 the doubling time is forecasted to be less than 3 months. It is simply no longer possible to “know†all of medicine or even a lot of medicine. So an old-fashioned, all-day, memorized test seems the height of anachronistic ridiculousness.
Many have argued that the test should be scrapped, and we should simply do the open-book online modules on a regular basis, which are more in line with the reality of learning in an information-saturated environment. Last year, the American Board of Anesthesiology junked its decennial exam in favor of weekly open-book quizzes.
But other specialties have yet to follow suit. So a plethora of groups are calling for a wholesale dismantling of the MOC system, arguing that board-certification-industrial complex amounts to little more than a money-hungry power grab. Groups like Change Board Recertification and Physicians for Recertification Change contend that ABIM and other specialty boards are not so subtly morphing their certifications into a requirement of medical practice (like medical licenses). These boards will have a monopoly on a captive audience who will be forced to pay whatever is asked. (And these costs don’t even include the thousands of dollars for books and courses that is pulled in by the extremely lucrative “board review†cottage industry, plus the many lost work days for both studying and the exam itself.)
For most docs, board certification is an expectation of employment. Certainly for those of us who work in large hospital systems or academic medical centers, it is an absolute requirement.
And so, for me and my fellow doctors who finished residency in a year ending in a 6, there is an exam looming this year.
A few months ago, I bit the bullet and paid off the balance on my $1940 ABIM fee. I signed up to take my recertification exam on October 7th, the last possible date in 2016 that I could swing. It was now official and I could procrastinate no more.
Studying for the boards is a bit like stuffing your face at a hotdog-eating contest: The first few hundred pages are intriguing and tasty; the medical facts seem highly relevant and you are going to be a better doctor for your patients. The next few hundred pages are interesting, but your brain is feeling sluggish. The few hundred pages that follow find you stuporous, and the facts slide gelatinously by. The remaining thousand pages are just confettied sauerkraut delivered by dump-truck onto a comatose slop of neurons.
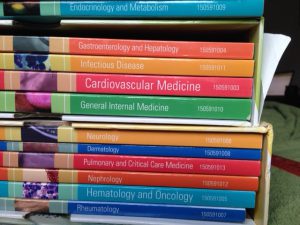
I figured I’d approach studying like I do with patients. I’d start with the vital signs. Height: 8 inches Weight: 20 lbs. Blood pressure cuffs did not fit around the stack. All told, it’s about 2,000 pages to assimilate.
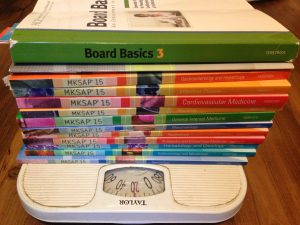 (Astute MOC veterans will recognize in the photo that these review books are not the most recent, but I just couldn’t bring myself to shell out $669 for the current set, so I gratefully accepted a hand-me-down set from a shell-shocked colleague who’d just finished her miserable 6 months of studying.)
(Astute MOC veterans will recognize in the photo that these review books are not the most recent, but I just couldn’t bring myself to shell out $669 for the current set, so I gratefully accepted a hand-me-down set from a shell-shocked colleague who’d just finished her miserable 6 months of studying.)
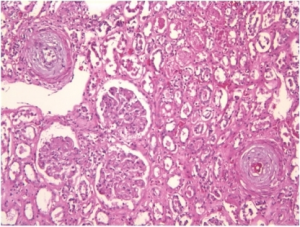
I picked a book from the stack at random: Nephrology. Last time I took the boards, someone warned me that scleroderma renal crisis was definitely on the test. Never mind that this is an exceedingly rare complication (renal crisis) of a very rare disease (scleroderma), and that treatment would absolutely by the purview of a specialist not a general internist.
Never mind that I’ve never seen a case in practice. I dutifully memorized the treatment (ACE-inhibitors), so should I end up shipwrecked on a desert island without any access to a textbook or database but with a companion who happens to erupt in scleroderma renal crisis, I will know exactly what to do (provided a bottle of ACE-inhibitors happens to wash up on shore along with us).
Six months ago, I was headed out of town for a conference, so I slid the nephrology book into my carry-on bag, gamely reassuring myself that I would study in the airport, or on the plane, or in the taxi.
Three days later, my trip was interrupted by an earth-shattering announcement from ABIM. After long consideration and debate, the ABIM would now offer ongoing open-book modules as an alternative method of recertification, though doctors may still choose the sit-down exam. (In a poll of ABIM diplomats, just 20 percent said that the exam would remain their preferred recertification method.)
Talk about the second coming! Hosannas could finally be sung. I tossed my untouched review book to the bottom of my suitcase, yodeling an off-key version of “ding-dong the test is dead.†I rummaged through the hotel room’s mini-bar, for something suitably celebratory—scrapping that miserable test and all that memorization was worth the inflated price for a small bottle of bubbly.
But then I read the fine print, and abashedly returned the champagne to the mini-fridge. The new open-book option would not begin until 2018. Those suckers who graduated residency in years ending with sixes or sevens would still have to take the exam, even though it had been recognized as obsolete. I looked at the nephrology book, pathetic and dog-eared from previous owner’s misery, and I felt the first symptoms of what I could only assume was scleroderma renal crisis.
I contacted Richard J. Baron, the President and CEO of ABIM. We had communicated once before over the issue of recertification and I learned—in full disclosure—that he not only trained at Bellevue Hospital (where I also trained, and where I currently work) but is also a charter subscriber to the Bellevue Literary Review, which I edit. Baron was gracious and unfailingly polite, despite our disagreements.
He acknowledged that the trend in education is away from the heavy-duty memorization tests, but ABIM still stands by their traditional 10-year exam. “Our exam is a state-of-the-art exam with an extraordinary amount of analytics and psychometrics behind it,†he said. “We’re not walking away from it.â€
I suggested to Baron that since things are finally changing, perhaps there ought to be a 2-year moratorium on recertification until the more humane option is available. “I completely understand that this can feel unfair to people in your situation,†he wrote to me in an email. “Making change always creates discontinuities, and I realize that is inevitably challenging.â€
‘Challenging’ is a charitable spin on the situation.
I briefly considered a civil disobedience protest—simply refuse to take the test and see what happens. But I checked with my hospital, and my medical privileges would be promptly suspended. That would not be helping my patients. So when September rolled around, I reluctantly pushed aside everything else in my life. The review books travelled with me everywhere, and I crammed whenever I could.
Now that it’s October 7th, I’m sitting in a windowless exam room, plowing through hundreds of multiple-choice questions. Will this will actually make me a better doctor? Will my patients derive benefit from this ordeal? I’m not sure.
But when scleroderma renal crisis shows up at my door, I’ll be ready. (from Slate.com)