Ethical Implications of Incidental Findings
 by Danielle Ofri
by Danielle Ofri
The Atlantic
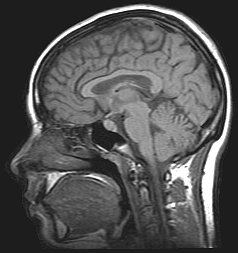
Imagine you are a medical student, volunteering in a research study to help out a friend. The fMRI during a memory test also happens to pick up a life-threatening aneurysm. Instead of starting classes, you are rushed to the OR. The fMRI’s “incidental finding” saves your life.
Or, imagine you are a marathon runner who pushes a little too hard, and collapses from dehydration and exhaustion. The ER staff, being thorough, does an MRI, and a brain tumor is “incidentally noted.” It’s a slow-growing type, the kind that may never be a real risk. But the surgery to remove it surely does pose risk. You and your doctor choose to wait, doing yearly scans to keep an eye on your own personal sword of Damocles. Your life is now haunted by an incidental finding.
Incidental findings are medical results that you weren’t looking for. The x-ray done for lower back pain that uncovers a spot on the liver. The urinalysis done to rule out cystitis that reveals trace protein in the urine.
At first blush, these seem like intrinsically good discoveries—potentially serious illnesses that get uncovered early. But plenty of spots on livers and protein deposits in urine are benign, while the tests required to determine that may not be.
Early this year, I wrote an article about one of my patients with chronic abdominal pain who visited the ER of another hospital. The doctors there—who were not familiar with her decade of dyspepsia—ordered a CT scan. Her stomach, gallbladder, intestines and liver were all in pristine condition, but “incidentally noted,” the report read, “was a 2-centimeter adrenal mass.” These adrenalomas are almost always benign, and almost always found only incidentally. They even have their very own appellation—he incidentaloma.
Nevertheless, I felt boxed into a clinical corner, forced to order expensive and complicated tests to rule out the minute chance of malignancy. The arduous process completely overwhelmed and panicked the patient, and we were never able to get to the actual diseases that she already had—diabetes, depression, and arthritis.
Two months later, I found myself in a Washington D.C. conference room, testifying before a razor-sharp committee of academics from law, nursing, medicine, philosophy, ethics, divinity, research, and government. This was a Presidential Commission for the Study of Bioethical Issues panel on incidental findings. The ethical considerations of incidental findings turned out to be much broader and more intriguing than I, as a ordinary primary care doc, had ever imagined.
In clinical medicine, we worry mainly about things that are uncovered when we doctors order tests and find other things—that’s what happened to my patient. It turns out that incidental findings are hardly incidental—they turn up in about a third of CT scans. In the case of abdominal CTs for trauma patients, the number of incidental findings can supersede that of trauma findings, and follow-up is notably spotty. In this age of defensive medicine, routine MRIs, and bundled tests, incidental findings are a daily occurrence.
But there are two other areas in which incidental findings are of escalating concern: research trials and direct-to-consumer medical testing.
Biomedical research is critical to the advancement of medicine, and the unsung heroes are the legions of volunteers who submit to all manner of investigation, mainly for the benefit of society, rather than themselves. But these countless lab tests, CT scans, and MRIs done for specific research questions are as prone to incidental findings as tests done in the clinical world, and pose unique ethical dilemmas.
For example, when a CT is ordered in the clinical world—as for my patient—a trained radiologist evaluates every aspect of the CT, no matter what the initial reason for the scan. But in the research world, these CTs might be of a low resolution, designed to focus on the particular research question, and often interpreted by a research scientist trained to examine just that one thing.
Are research scientists obliged to have a radiologist thoroughly evaluate each scan? Are they obliged to use the high-level resolution scans on par with those in the clinical world? These technicalities may seem like hair-splitting, but they could be prohibitive enough to cancel a research study.
And what happens when an incidental finding is noted? Are researchers responsible for obtaining medical care for the volunteer? Are they financially responsible for such care? Can there be any malpractice implications, especially for researchers who are also MDs?
The situation gets even murkier when it comes to direct-to-consumer (DTC) medical testing. The development that has brought these ethical controversies to the forefront is the advent of low-cost whole-genome sequencing. In the past, sequencing an entire genome was a laborious, expensive endeavor that was limited to major research labs. Now, companies have sprung up to offer personal sequencing. Just send a bit of saliva and $99—shipping and handling included—and you, too, can have the entire contents of your DNA laid out like a take-out menu.
At first glance, this sounds straightforward. But it isn’t. What should be done if the test discovers a gene for a serious, heritable illness ? In the clinical setting, there is a trained genetic counselor to work with a patient and the results, but with direct-to-consumer testing, a person is largely on their own. Does the company have an ethical obligation to make a referral for treatment? To inform family members who might also be at risk? What happens if the results show a chromosomal sex that is different than the person’s known sex? What happens if testing reveals parental lineage that isn’t what was expected? And what happens if the tests are wrong?
The bioethics commission listened to testimonies from doctors, patients, researchers, and DTC companies. They heard cases in which incidental findings led to life-saving results, and cases in which incidental findings led to unnecessary pain, fear, and cost.
The main conclusion of the commission was that incidental findings aren’t incidental at all. Some are so prevalent that they should be anticipated. Not that any one doctor could anticipate any one incidental finding on any given patient, but that all patients, research subjects, and DTC consumers should be routinely warned of incidental findings. Standard consent forms should emphasize that incidental findings are the norm and should be expected.
If doctors, researchers, and DTC companies have a plan in place to deal with incidental findings, they won’t have to scramble when it happens—which is what happened with my patient and me. Our incidental finding felt like an unexpected clinical bomb that elbowed everything else to a second tier.
The final report published by the commission, released today, is entitled “Anticipate and Communicate, and offers suggestions for how to prepare for incidental findings, including discussing the risks and benefits with patients, and including information about the possibilities of incidental findings within standard consent forms.
Before I presented to this commission, I’d viewed incidental findings as minor annoyances that pop up every so often. Now I think of them as part and parcel of everyday medicine. Whenever I send a patient for CT or MRI, I mention the possibility of unexpected findings. And although the term “incidental findings” has a charming ring to it—zingy enough for me to have chosen it as a book title some years back—I’ve decided that I will retire the phrase. Findings are findings—whether you sought them or not. Once you have a finding on your hands, it’s only how you ended up there that is incidental.
