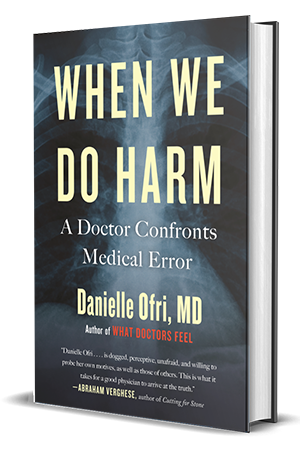
AJN review of “When We Do Harm”
by Theresa Brown
American Journal of Nursing
Danielle Ofri’s When We Do Harm: A Doctor Confronts Medical Error (Beacon Press, 2020) hits like a punch to the gut, but I actually felt calmer about errors when I finished the book, because Ofri insists that errors are inevitable: health care is performed by human beings, who all make mistakes. As clinicians and as members of health care institutions, how we handle errors in clinical practice is what really matters. Our job, as Ofri emphasizes throughout, is to keep patients as safe as possible.
Nurses will appreciate the book’s epigraph, an apt quotation from Florence Nightingale: “It may seem a strange principle to enunciate as the very first requirement in a hospital that it should do the sick no harm. It is quite necessary, nevertheless, to lay down such a principle.” Nightingale wrote this in 1863; that it continues to be relevant to contemporary practice strikes me as quite sad.
In the nearly 150 years since Nightingale made her plea for safer hospitals, health care has become unbelievably complex, fragmented, profit focused, and high tech. Ofri argues that these factors, in combination with the use of electronic health records (EHRs), put patients at risk in innumerable ways.
The book begins with a discussion of the work of physician and patient safety expert Lucian Leape, who studied data from the 1984 Harvard Medical Practice Study and concluded that almost all medical errors resulted not from individual mistakes, but from system failures. For example, a nurse giving the wrong medication might seem like one person’s mistake, but analysis almost always revealed a cascade of system errors behind that singular mistake.
The case of pediatric patient Pablo Garcia illustrates this point well. The resident taking care of Pablo at the University of California, San Francisco, Children’s Hospital used the EHR system to order 160 mg of the antibiotic Bactrim for Pablo, based on his weight of 38 kg. A pharmacist confirmed this dose, but when the resident reconfirmed the order, the computer defaulted to mg/kg for the dosing parameters, upping Pablo’s dose to 6,160 mg, or 38½ tablets of Bactrim. The robot that dropped off the drug verified that the dose had been double-checked by the pharmacy. Pablo’s nurse initially balked at the amount of Bactrim ordered, but was reassured by the recorded double checks and was under great pressure to deliver medications on time. The nurse gave the dose. Shortly afterward, Pablo began seizing, then went into respiratory arrest. A code was called and he was resuscitated, miraculously with no lasting physical or cognitive damage.
I imagine that nurse and resident have never forgotten that day, and still carry the terror and shame of that mistake with them. Yet such intense personal reactions to error can have a strong pedagogical effect. As Ofri explains, “Once an emotional component is tied into an experience, it is remembered much more intensely and intuitively.” We can learn from the mistakes that scare us the most, and this will make us better clinicians.
Nurses will like this book because Ofri approaches medical error as an issue that physicians and nurses own together. Furthermore, she champions nurse advocacy as essential to preventing errors. Describing the work of Peter Pronovost, a physician who developed a medical checklist for use as a patient safety tool, Ofri states, “What might ultimately be considered the secret sauce of Pronovost’s original checklist was . . . that nurses were empowered to speak up. This was a culture shift of epic proportions.”
It’s significant that the phrase “culture shift” recurs in When We Do Harm. Ofri insists that medical errors will lessen only when the culture of health care shifts away from one characterized by clinicians frantically typing into computers and hurrying through patient encounters, and back to one wherein all hospital staff actually talk with and listen to one another.
To prevent mistakes, Ofri argues, health care workers need time and space to think. Patients need our uniquely human ability to analyze and reason: “It’s easy to make a checklist for how to evaluate a fever . . . but you can’t checklist clinical thoroughness, good listening, effective communication, intellectual humility, or professional responsibility.” All patients deserve the safest care possible—and that’s exactly why we nurses and physicians must be empowered to be the most thoughtful and careful clinicians we can be.